Highs and Lows
A rough night
1am
Hannah wakes up as she needs the toilet. Complains of pain…in her chest but also her right shoulder when breathing in.
I get her back into bed. ..almost bolt upright as she says it hurts too much otherwise.
She probably hardly got any pain relief at her last dose before bed as she threw up and couldn’t repeat the dose as there was no way of knowing what she’d kept down.
The nurse asks what she wants to do as she can’t have any more paracetamol for a few hours.
“Don’t want morphine” is Hannah’s immediate reply!
She can’t have anything else yet, but she’s adamant she’ll wait until her next dose of paracetamol. When the nurse asks how much it hurts on a scale of one to ten, she says 7. Nurse asks again if she’s sure she doesn’t want morphine and Hannah says she’s sure.
Whilst I don’t wish her to suffer unnecessarily, I admire her stoicism and determination.
3am
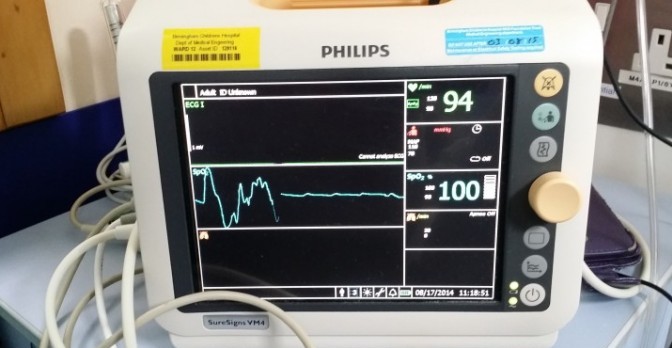
Hannah went back to sleep and when nurse came in to check on her she said her resps (respiratory rate) were down and heart rate was down when she was asleep, so no worries.
Hannah just woke up and asked for my help to get out of bed and get to the toilet. I’m sure she doesn’t really need the toilet but is waking up in pain and uncomfortable and the toilet is the most natural / spontaneous response.
I ask about the pain. She says “it’s not better” and rates it a 6/10.
4am
Wakes up in pain again but manages to settle down on her side with bed head lowered again
4.50am
Pain and discomfort. Wants to sit up in bed again. Says her chest is making strange noises and she doesn’t like it.
“Weird bubbly sound” above her wound, where we kept seeing the rising dome on exhale. Is it the Pneumothorax?
5.15am
Wants to lie back down on her side. Pain still the same.
6 am
Making lots of little moaning noises.
“I don’t like it”.
Can’t get comfortable.
Nurse brings antibiotic tablet and paracetamol. Hannah takes first paracetamol and throws up lots of bile. The tablets are stimulating her gag reflex. She had an anti-emetic drug (to stop her throwing up) written up but only to be given intravenously (IV). Nurse says she’ll get her written up to have it orally.
The nurse says the noises Hannah can hear are the surgical emphysema. What surgical emphysema??
6.50am
Now sitting up in bed catching up on Facebook. Haven’t dared getting her to try taking the other 2 tablets yet. At least Facebook is distracting her a bit and she’s calmer again. Heart rate, resps and blood pressure have come back down.
7.10am
Nurse just came back in. She said surgical emphysema isn’t documented in her notes anywhere. I told her we’ve mentioned the bubble rising on her chest above her wound numerous times. Every nurse has picked it up and mentioned it to the doctors. The doctors have felt the crackles (subcutaneous crepitation, also known as ‘creps’) and there’s been vague mention of it being related to the Pneumothorax, but nobody has mentioned the term surgical emphysema before. The nurse said she’s told the doctor and it’ll get flagged up to the registrar. It should get documented in the notes.
Nurse confirmed it should clear by itself over time.
7.30am
Hannah has managed to take and keep down the rest of her tablets. Her pain level has improved a little.
I’ve turned down her oxygen to half a litre and her Sats are still at 100%. The process of weaning her off the oxygen is going well.
9.45am
Hannah had a reasonable breakfast…not many Coco pops but 2 cups of chocolate milk and some Lindor chocolates…then promptly threw it all back up while having a walk down the ward!
It’s horrible to watch her go through all this 🙁
She keeps improving on her breathing exercises though. Her walking is better each time and her voice is getting stronger.
She is getting better. She is on only minimal oxygen and her Sats are very good, so she may be off it by tonight. Her walking and general mobility keep improving. We are getting there, but this is the difficult stage where she needs to do all the work while she’s exhausted and in pain. 🙁
And I need to make sure I don’t fall over while helping her in the shower etc as I’ve now started swaying!
Have gone back to parents’ accommodation for a shower…then back to the ward for ward rounds and I’ll come back to our room this afternoon for a nap.
11am
Aaaargh! Ward rounds were early today and I missed them. Anyway…they’re happy with everything and it’s up to Hannah now how fast she gets well enough to go home.
They’ve turned off her oxygen and she was saturating at 98 while fast asleep. Now, after walking up & down the corridor twice, she’s at 100% That’s just showing off! Hehe
She’s sitting in her chair, watching TV and actually laughing! 🙂
12.45pm
The brilliant (even if I say so myself) French plaits I did pre-op on Tuesday morning are out and hair is brushed. There were basically NO knots, so the plaits worked 🙂
My babychick is back…she’s been really chatty, had a reasonable portion of roast dinner and laughed at the TV. 🙂
And she’s back to giving me one of her ‘looks’ for insisting on taking a pic lol
Here’s a picture of her ‘incentive spirometer‘ for her breathing exercises…showing how much progress she’s made since Friday afternoon! 🙂 She has to raise the base inside the chamber when breathing in…Ideally all the way to the top. Friday she barely shifted it. Now, she’s taking in almost 1.75 litres of air with her deep breaths. She has to do 10 repetitions every hour and I’m a worse drill sergeant than the ‘physio terrorists’…I won’t count a breath unless it’s at least as high as her previous best!
A fabulous afternoon
As the day went on, Hannah got better and better, walking really well, especially without an oxygen tank for one of us to carry around after her, and kept improving on her breathing exercises. It started to feel like we had the old Hannah back!
We got permission to take her off the ward so we went to the hospital’s garden for a wander and a sit-down in the sun and fresh air. It was great!
We took the obligatory selfies:
Charlie then arrived with Sue (Simon’s mum) and Lauren (our niece), so Simon and I went into town for our lunch, leaving Hannah in great company.
When we got back, they looked like they’d had a great time – they watched DVDs and chatted…and Charlie and Hannah were snuggled up on Hannah’s bed together. Lovely to see! 🙂
6pm
Hannah’s had some pain at the bottom of her ribcage, both sides. Over the last hour or two, she’s started looking worse and struggling with her breathing exercises and taking decent sized breaths in general.
Doctor has taken a look, put her back on oxygen and ordered an x-ray. He thinks her Pneumothorax has re-appeared / got worse. I thought Hannah’s recovery from heart surgery was going far too smoothly this time, compared to our previous experience!
Two steps forward…one step back … That’s still forward movement / progress. Overall we’re still getting there, just maybe not quite so fast.
Comedy moment today:
As I’m speaking to Hannah; she can’t hear me because she has her iPod on and earphones in. She says “pardon?” while pulling her oxygen cannula out of her nose!
8pm
Doctor discusses X-Ray results with us. It appears the same Pneumothorax that seemed to have gone before is still there, though no worse than before. Seems Hannah just needs more time for it to dissipate naturally. She needs to stay on oxygen and also carry on with lots of mobilisation (moving around, walking etc) and with her breathing exercises.
She’s been on extra oxygen since the Doctor came to see her earlier and she seems better for it – more comfortable and in less pain (she’d managed, earlier, a peculiar combination of pink lips with high O2 Sats and looking grey-skinned at the same time!).
Next to the Doctor stood the on-call surgeon in his scrubs. I nearly had palpitations before the Cardiology Registrar started speaking to update us! The surgeon did add, however, that if things deteriorated, they’d have to take her into theatre and insert a drain to clear the air out of her chest. I knew that was a possibility but really hope it doesn’t come to that. Poor Hannah!
I’m keeping everything crossed!
10pm
I went back to parents’ accommodation once we’d had the Doctor’s update re the X-Ray. I’ve had some dinner, got changed into comfy PJs and updated the blog as well as friends & family.
I’m now going to have an early night and attempt to sleep, as last night was exhausting and we don’t know what lies ahead that we may need our energy for.